The Basics of Vestibular Care
By guest blogger Dr. Madison Oak, DPT
Vestibular Rehabilitation Therapy is a very niche practice within physical therapy focused on treating the inner ear. In elementary school, we learn that the ear is for hearing, but what we often forget is that it is also an essential part of balance, stability, and equilibrium. There are many conditions that can present with symptoms of dizziness that stem from the inner ear. These include:: Benign Paroxysmal Positional Vertigo (BPPV), Meniere’s Disease & Secondary Endolymphatic Hydrops, and Vestibular Migraine. Each of these, and more, occur when your vestibular system is dysfunctioning and cause dizziness, vertigo, and lightheadedness. Let’s jump into the hows and why’s of vestibular dysfunction!
Inner Ear Anatomy and Pathology:
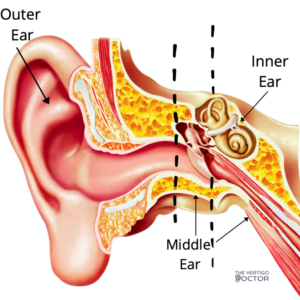
The inner ear is located deep within your skull; you can see in the picture below the outer, middle, and inner ear. The outer ear is the part you can see outside your head and proceeds to the space the doctor looks in when you have an earache. The middle ear begins at your tympanic membrane (ear drum) and extends through to your eustachian tube, which connects your ear to the back of your throat. The inner ear is placed deep in your skull, in the direction toward your brain.
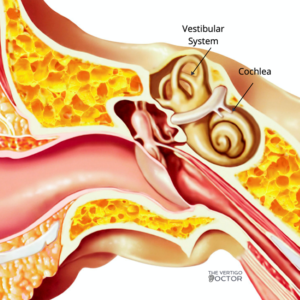
Within the inner ear, you have two sections, the cochlea and the vestibular system. Your cochlea is the hearing organ, the curly- shaped part that almost looks like a snail. The vestibular system is the other circular structure, made up of the otolith organs and 3 semicircular canals. Together these two control your balance, stability, and equilibrium; when one part of this system experiences dysfunction, you can experience imbalance, lightheadedness, anxiety, and vertigo.
Common Vestibular Diagnoses:
There are many vestibular diagnoses, some being more common than others, that we think of when it comes time for a differential diagnoses. The most common vestibular diagnoses are Benign Paroxysmal Positional Vertigo and Vestibular Migraine, but there are many others. Knowing the key differences between each kind of dysfunction is vital for diagnosis and treatment.
Benign Paroxysmal Positional Vertigo:
Benign Paroxysmal Positional Vertigo, abbreviated BPPV, is the most common cause of true spinning vertigo (1). BPPV is defined by episodic vertigo lasting 10-30 seconds and is evoked by specific head positions. BPPV occurs when tiny calcium-carbonate crystals, called otoconia, become dislodged from the otolith organs where they’re held in your inner ear, and end up in your semicircular canals. [In order to picture this, go back to this lesson on ear anatomy!] This causes the perception of room spinning or wall sliding. Benign Paroxysmal Positional Vertigo is a long name that really spells out what it is.
- Benign: non-harmful, dangerous
- Paroxysmal: sudden, short-term
- Positional: occurring in specific positions
- Vertigo: true spinning dizziness
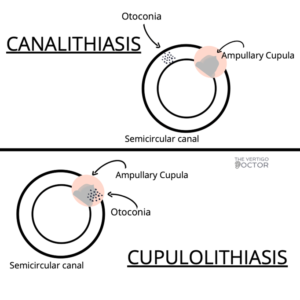
When you turn your head into certain positions, typically laying down at night to go to sleep, rolling over in bed, or looking up into a cabinet, the otoconia move inappropriately within the semicircular canals where they do not belong and cause repetitive, uncontrolled eye movements, called nystagmus. The nystagmus is what causes the room to look as though it’s spinning, your PT will look at the nystagmus and determine which canal and type of BPPV you have. BPPV can be classified into two types: canalithiasis, where the otoconia are trapped in the semicircular canal, and cupulolithiasis, where the otoconia are trapped in the ampullary cupula. This is pictured below:
Once diagnosed, BPPV should be treated by a physical therapist; it can usually be cured in 1-2 sessions. The first will be diagnosing and treating the canal where the otoconia are located, and the second is to recheck the affected canal and other canals where otoconia are located. The treatment for BPPV is a Canalith Repositioning Treatment (CRT), and shoudl only be performed with a qualified healthcare professional. Call your physical therapist or primary care provider to find out if they are able to help you find the care you need.
Secondary Endolymphatic Hydrops & Meniere’s Disease:
Ménière’s Disease and Secondary Endolymphatic Hydrops are chronic, frustrating, and incurable inner ear diseases thought to be caused by a buildup of endolymph in the membranous labyrinth of your cochlea and vestibular system (2). This buildup of endolymph causes swelling on the membranous divide between the endolymph and perilymph, the Reissner’s membrane. This imbalance in your vestibular system causes symptoms of vertigo, spinning, dizziness, hearing loss, and tinnitus. The potassium-rich endolymph flows into the perilymph, causing your symptoms to occur until the membrane heals, and/or the fluid balance is restored (2). Ménière’s Disease is also called Primary Endolymphatic Hydrops. Primary and Secondary differ as Primary Endolymphatic Hydrops (Ménière’s Disease) is believed to cause a full rupture of the Reissner’s membrane, creating intermittent and/or sustained hearing loss, and Secondary does not.
Primary and Secondary Endolymphatic Hydrops are usually triggered as a response to an underlying condition. These conditions include, but are not limited to, surgeries that affect the inner ear, inner ear infections, allergies, and head trauma (3, 4). The attacks are spaced weeks to months apart, and over time can slowly destroy your vestibular and hearing systems. These symptoms manifest in different ways depending on the individual. Regardless of your symptoms, we need to treat the symptoms and the underlying condition simultaneously to preserve your vestibular system and restore homeostasis in your body. Treatment for these conditions are based in lifestyle modifications and dietary changes. Patient’s can avoid symptoms recurring by monitoring what they eat, drink, and do!
Vestibular Migraine:
Migraine is a genetically induced hypersensitivity to internal or external stimuli within central nervous system neurons (5). When a neuron that is primed to a migraine is triggered by a stimulus either inside or outside of your body, the neuron reacts through a migraine (5). Migraine is generally considered a headache, however not everyone with migraines experience headaches. Some people get migraines in the form of vertigo, called Vestibular Migraine or Migraine Associated Vertigo. It is estimated that about 1% of the population has Vestibular Migraines (6). Because Vestibular Migraine’s diagnostic criteria are new, it often goes undiagnosed or misdiagnosed for a while before an individual receives a diagnosis. Patients are sometimes alternatively diagnosed with Ménière’s Disease or chronic BPPV instead of Vestibular Migraine, Some of the symptom and diagnostic criteria will be helpful to pinpoint exactly what’s going on for you. People who experience Vestibular Migraine fit the following criteria:
- At least 5 episodes of vestibular symptoms of moderate or severe intensity lasting 5 minutes to 72 hours
- Current or previous history of migraines with or without aura according to the ICHD classification
- One or more of the following migraine features with at least 50% of vestibular episodes:
- Headache with at least 2 of the following characteristics: One-sided location, pulsating quality, moderate or severe pain intensity; photophobia or phonophobia
- Visual aura
- Not better accounted for by another vestibular or ICHD diagnosis
Once you or a loved one is diagnosed with Vestibular Migraine, there are many treatment options. There is not a quick fix formula for Vestibular Migraine, and finding what works for you may be a process. It is important to remember that you have to treat the migraine first, and the symptoms related to the migraine second. A neurologist or migraine specialist is best suited for your needs as a migraine patient, and a vestibular physical therapist is the best practitioner for the feelings of dizziness, lightheadedness, and nausea. Working with a healthcare team, instead of just one provider, is an excellent choice when it comes to treating Vestibular Migraine.
Anxiety Related Dizziness:
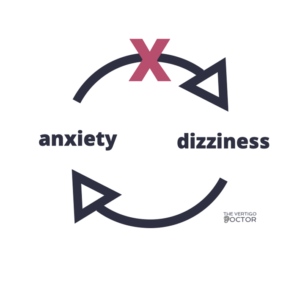
Anxiety related dizziness is an under diagnosed and under treated reason people feel lightheaded, imbalance, and fearful of walking. Anxiety can be an underlying cause of dizziness or related to another diagnosis. Having any form of dizziness can be incredibly anxiety provoking, and the two factors work together to make you feel worse. They react in a cycle, anxiety making you dizzy, and the dizziness making you anxious. Treating anxiety related dizziness is multifactorial. Cognitive behavioral therapy, physical therapy, and psychiatry can work hand-in-hand to make you or your patient’s symptoms retreat and disappear. Treating both the anxiety and the dizziness simultaneously is important to returning to function and feeling like yourself again.
Treatment:
Treating vestibular dysfunction is very similar to other physical therapy treatments. Your PT will take subjective and objective measures to determine what is difficult for you, why you are dizzy, and what your goals are. You will work with your PT to come up with a home exercise program that fits your specific needs, and will potentially work with you to make some lifestyle and dietary changes in order to prevent future vestibular episodes. Whether your symptoms are true vertigo from a mechanical issue like BPPV, or the feeling of nausea and lightheadedness from Vestibular Migraine, your vestibular PT will be able to help you recover faster.
Sources:
(1) Fife, T. D. (2017). Dizziness in the Outpatient Care Setting. CONTINUUM: Lifelong Learning in Neurology, 23(2), 359-395. doi:10.1212/con.0000000000000450. https://journals.lww.com/continuum/Fulltext/2017/04000/Dizziness_in_the_Outpatient_Care_Setting.7.aspx
(2) VEDA. (2020, June 24). Ménière’s Disease. Retrieved September 01, 2020, from https://vestibular.org/article/diagnosis-treatment/types-of-vestibular-disorders/menieres-disease/
(3) VEDA. (2020, August 07). Secondary Endolymphatic Hydrops (SEH). Retrieved September 01, 2020, from https://vestibular.org/article/diagnosis-treatment/types-of-vestibular-disorders/secondary-endolymphatic-hydrops-seh/
(4) BC Balance and Dizziness. (n.d.). Secondary Endolymphatic Hydrops. Retrieved September 01, 2020, from https://balanceanddizziness.org/disorders/vestibular-disorders/secondary-endolymphatic-hydrops/
(5) Rothrock, J., MD. (2020). What is Migraine? Retrieved September 02, 2020, from https://americanmigrainefoundation.org/resource-library/what-is-migraine/
(6) Tepper, D. (2015, November 12). Migraine Associated Vertigo. Retrieved September 02, 2020, from https://americanmigrainefoundation.org/resource-library/migraine-associated-vertigo/
About Dr. Madison Oak, DPT

Dr. Madison Oak is a Vestibular Physical Therapist based in Manhattan, New York who specializes in treating dizziness and vertigo of all kinds. She graduated with a clinical Doctorate in Physical Therapy from the University of Wisconsin and has been treating patients with dizziness ever since.
Dr. Madison Oak understands that dizziness comes in many forms, from vertigo to lightheadedness, and knows that finding the source of your dizziness is the best way to treat it. Finding the root of your problem, and treating the whole person, instead of just the symptoms, is very important to her. That’s why she started TheVertigoDoctor.com; to provide easy to read, accessible, resources to patients who are dizzy and struggling to find diagnosis, prognosis, and treatment. She strives to help her patients reach functional goals to return to a dizzy-free way of life.
Categories
-
Recent Posts